Education
How to Get Rid of Hormonal Acne


SHARE
Education
How to Get Rid of Hormonal Acne
Medically reviewed by Aimee Paik, MD
Written by Apostrophe Team
Last updated 11/3/2024
How to Get Rid Of Hormonal Acne
It’s the morning of your big date, two hours before your big presentation, or even your wedding day, and suddenly your chin has a new friend—a big, red cyst.
If you’re experiencing a cyst right now, you’ve likely had one in the past, too. You’ve probably even taken steps to address your acne, only to find that each new acne treatment from cleansers to creams comes up short.
With all the misinformation on skincare, it’s normal to take a few detours down the wrong path.
The good news? Now, you’re in the right place! Our skincare experts have a full rundown on everything you need to know about hormonal acne and, most importantly, how to treat it.
What is Hormonal Acne?
Pop quiz: what is acne? To start, not every pimple is created equal. In fact, we can count six different kinds:
Open comedones, also known as blackheads
Closed comedones, alias whiteheads
Papules
Pustules
Nodules
Cysts
To understand the causes of and solutions to these six unwanted visitors on your face, we first need to understand what acne is.
Let’s break down the four leading causes of acne:
1. Increased Oil Production – One of the causes of acne, especially hormonal acne, is an increase in sebum, or oil, production caused by an increase in androgens. Androgens are male sex hormones found throughout the bodies of both women and men. Androgens regulate oil production in the skin, so an increase in androgens can cause too much oil to build up, blocking the pores and causing acne. It also provides a great environment for bacteria to grow... we’ll get to that later.
2. Dead Skin Cells – Keratinocytes are the primary type of skin cell. Throughout their life, they move up through the layers of your skin until they reach the surface and shed. These skin cells also produce a tough protein called keratin. In a process called keratinization, these dead skin cells clog your pores rather than shedding.
3. Inflammation – Acne is principally a skin disease of chronic inflammation. That’s no surprise to anyone who has dealt with swollen, painful cysts.
4. Bacteria – Cutibacterium acnes (c. acnes)) is a bacteria that lives in the human skin, including the sebaceous follicles on your face. It is linked to an inflammatory response that leads to acne, hence its name.
So what’s behind your zits?
Unfortunately, hormonal acne can be similar in appearance to the acne caused by plain-old clogged pores. But finding the right treatment depends on understanding the cause.
If your acne comes and goes with your period, it might be hormonal. Likewise, hormonal acne can result from changing hormone levels during pregnancy, perimenopause, and menopause. They might also fluctuate when you start or stop birth control pills.
The chin is a common place for hormonal breakouts. This type of acne can be especially frustrating because treating it requires a different approach than other types of acne.
For some cis-women, however, these hormonal imbalances are more severe as a result of endocrine disorders. The most common endocrine cause of hormonal imbalances is polycystic ovarian syndrome (PCOS). Women with PCOS suffer from hyperandrogenism. These excess androgens result in an overproduction of oil and, consequently, acne.
Up to 90% of women with hyperandrogenism have PCOS, so a trip to the gynecologist can also help if you believe your acne is hormonal. If you experience fewer than 9 periods per year and you have acne, you may have PCOS.
Does Hormonal Acne Go Away?
If you’ve ever dealt with hormonal acne, you know these aren’t the type of pimples that just disappear overnight with the help of a spot treatment and prayer.
Hormonal acne typically appears, flares up, and eventually disappears over the course of a few weeks.
Unfortunately, acne caused by hormonal imbalances is cyclical and will continue to invade your face again and again unless the underlying cause is properly addressed and treated.
What Triggers Hormonal Acne?
We’ve already established that hormonal acne is the result of hormonal imbalances caused by things like:
Menstrual cycle
Pregnancy
Perimenopause
Menopause
Birth control pills (starting or stopping)
Endocrine disorders (like PCOS)
But what causes flare-ups? The contenders are familiar.
Hormonal Changes
Women’s hormones are constantly changing, from major life events like pregnancy and menopause to their monthly menstrual cycle. Any of these hormonal changes can trigger flare-ups of hormonal acne.
If you menstruate, start tracking your cycle so you can identify when your hormonal acne is at its worst.
Stress
Stress exacerbation is one possible diagnostic criteria for acne in general. To take things a step further, stress causes a rise in cortisol levels, which is a hormone, deeming stress a cause of hormonal acne. Studies have linked acne and stress in adult women based on several proposed mechanisms.
Chronic stress can increase adrenal androgens and, consequently, oil production.
Stress also releases cortisol which triggers a chain reaction of hormones that increases oil production and inflammation.
Diet
Your diet can also trigger hormonal acne. For example, 100% pure chocolate was found to cause acne. Dairy is also often anecdotally linked to acne. While some studies show a positive association between dairy, particularly milk, and acne, the results are not conclusive.
The strongest evidence associates hormonal acne with foods with a high glycemic index, such as:
White rice
White pasta
Candy
Couscous
French fries
Sweetened fruit juices
High sugar food and beverages
These foods cause your blood sugar to spike, which, in turn, causes your body to release insulin. Insulin triggers other hormones that can clog pores, including androgens, growth hormones, and glucocorticoids.
Mistreating Your Acne
You’ve probably heard the advice never to touch your face.
While we all scratch our noses from time to time, more dramatic interventions can actually worsen your hormonal acne.
Improperly popping pimples can push more bacteria into the skin, leading to further inflammation. Over time, this could create scarring.
Trying to give yourself an at-home extraction could also damage deeper tissues, resulting in more deep cysts.
Likewise, regular breakouts can worsen hormonal breakouts. Combined, these risks make it incredibly important that you treat your acne properly.
What is the Best Hormonal Acne Treatment?
Now that you understand all the ins and outs of hormonal acne, you can choose the best treatment to conquer it once and for all.
One option is consulting a dermatologist. But whether you’re struggling to get an appointment or you’d prefer to do your own research, we’re here to help you understand the available treatments.
Hormonal Treatments
Hormonal treatments can address the underlying causes of hormonal acne.
Options include:
Androgen Blockers – Spironolactone is a medication that decreases androgens, which in turn decreases the size and activity of oil glands. Topical spironolactone is appropriate for people of all genders, while only women (cis- and trans) can use oral spironolactone.
Oral Contraceptives – Also referred to as birth control pills, contraceptives containing estrogen and progestin can treat acne in both adolescent and adult women. The FDA has approved three types of oral contraceptives to treat acne:
Ethinyl estradiol-drospirenone
Ethinyl estradiol-norgestimate
Ethinyl estradiol-norethindrone acetate
These pills have different brand names, so check with your doctor to confirm you’re starting a birth control appropriate to treat acne.
Antibiotic Treatments
Oral antibiotics are sometimes prescribed to treat moderate to severe acne and treatment-resistant inflammatory acne. The two most common acne-fighting antibiotics are:
Tetracyclines
Macrolides
Other types of antibiotics are also sometimes used to treat acne. Doctors often prescribe systemic antibiotics along with topical treatments like benzoyl peroxide or retinoids.
Topical antibiotics such as erythromycin and clindamycin are often used in conjunction with other treatments. Another form of topical antibiotic is called dapsone. It has both antibacterial and anti-inflammatory properties.
A Simple Skincare Routine
Once you’ve created a plan of action to address your hormonal acne, set yourself up for success with a good skincare routine featuring the following steps:
Cleanse twice a day with a gentle cleanser
Treat with retinoids, salicylic acid, or an Apostrophe topical formulation
Moisturize with a non-comedogenic lotion
Protect your skin with broad spectrum SPF 30+ sunscreen
From there, consistency is key. Keep taking any medications and applying topical treatments while practicing great skincare to experience improvement over time.
Your Answer to the Question: How to Get Rid of Hormonal Acne
Hormonal acne is an endlessly frustrating condition, but there is hope. Hormonal treatments, antibiotics, and topicals can help improve your acne and your skin’s long-term health.
Your journey to clear skin starts today with Apostrophe. Start a derm consultation online, and if prescribed, you'll receive a personalized skin care treatment plan crafted by an online dermatologist or provider within 48-hours. With Apostrophe, there are no office visits, no copays, and no trouble—just the right formulations for your skin.
Shop this post

Clindamycin
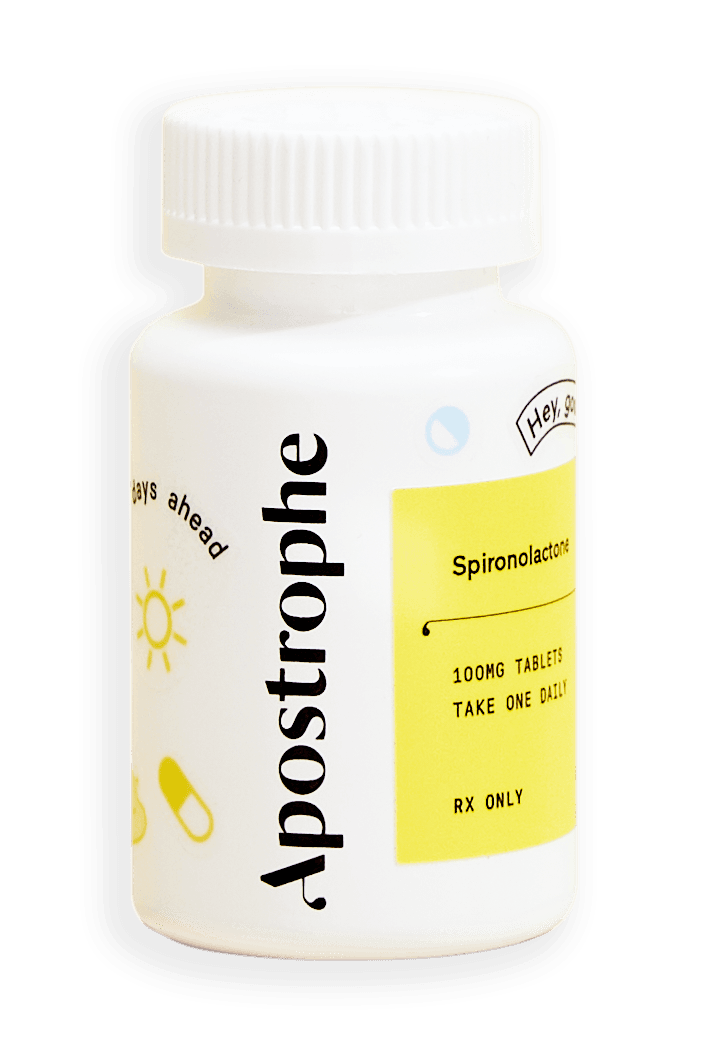
Oral Spironolactone

Topical Spironolactone

Tretinoin
Like what you just read? Sign up for our email list to get the scoop on skincare science delivered straight to your inbox.

Deep Dives
A dermatologist shares his thoughts on the recent studies about benzoyl peroxide and benzene.
Read More
Education
What is milia?
What is milia? Today, we’re jumping into one type of bump that you may have heard about most commonly in infants — milia.
Read More
Education
Best moisturizer for acne-prone skin
If you have combination acne-prone skin, figuring out which moisturizer is best for your skin might be tough. In this guide, we break down the best moisturizer for combination, acne-prone skin.
Read More
